Medicare telehealth reimbursements cover many services that practitioners perform at distant-site facilities for patients located at qualified originating-site locations. Claims for telehealth services rose from $61,302 to more than $17,000,000 between 2001 and 2015. The increasing popularity of these claims caught the attention of the Department of Health & Human Services, which engaged the OIG to review whether these claims complied with Medicare requirements. The OIG recently published a report detailing its audit of Medicare telehealth claims submitted to the Centers for Medicare & Medicaid Services (CMS) during 2014 and 2015. More than half of the claims distant-site providers submitted lacked a corresponding originating-site entry. Upon review of a sample of these deficient claims, the report discovered that a significant number were unallowable. The OIG concluded that CMS should have disallowed payment for more than 25% of the $13,795,384 in telehealth claims submitted during the period reviewed.
The lack of industry awareness regarding telehealth claim requirements was a major concern that the OIG identified in its report. When submitting telehealth claims, the three primary considerations that practitioners should address are whether
- the claimant is eligible to submit a claim;
- the claim includes covered services using approved telecommunications equipment; and
- the patient is receiving those services at a qualified originating site.
Federal statutes and the Medicare Claims Processing Manual describe which providers and institutions are eligible to submit telehealth claims and under what circumstances. CMS provides several useful resources that assist claimants in determining which services are covered and whether the patient is receiving services at a qualified location. Consulting these resources alone would have prevented most of the unallowable claims that the audit discovered.
Below is an analysis of the OIG Audit Report.
I. Unallowable Claims
Due to the vast increases in telehealth claims during the past 15 years, the OIG performed an audit and found that CMS reimbursed more than $3,600,000 in unallowable claims. The audit sampled 100 claims for telehealth coverage and found 31 that did not meet Medicare requirements.
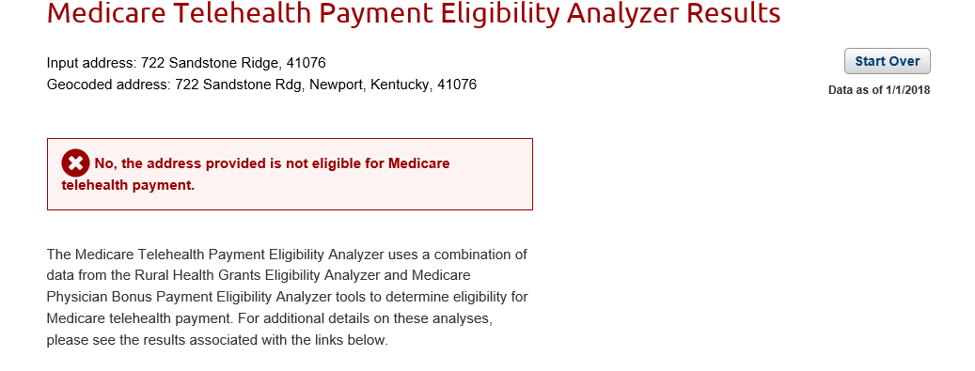
Non-Rural Originating Sites: Of those 31 claims, 24 were unallowable because the patients received services at non-rural originating sites. Providers can verify that the patient is located at an eligible originating site using the Telehealth Payment Eligibility Analyzer.
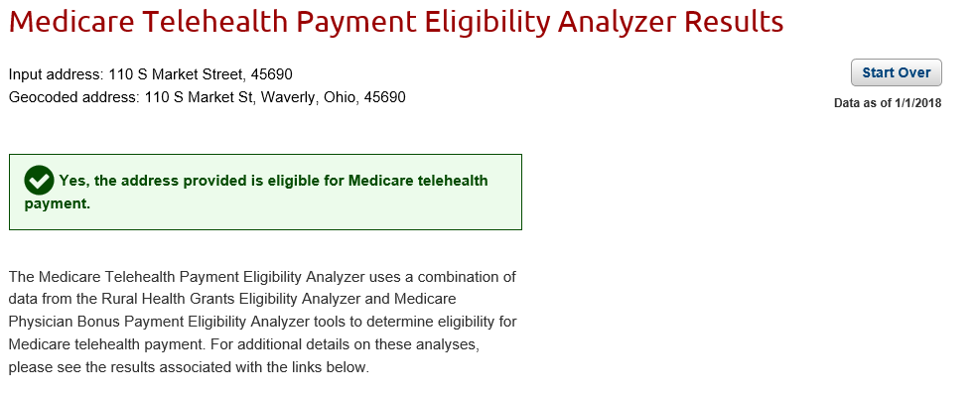
When visiting the Analyzer site, providers may enter the street address information of the originating site and receive confirmation whether it is eligible for reimbursement or not:
Or:
Ineligibility of Submitting Institution: There were seven claims that were unallowable because ineligible institutional facilities submitted them. Institutional facilities may bill Medicare for telehealth services only when
- the facility is a critical access hospital (CAH) that elected the Method II payment option and the practitioner reassigned his/her benefits to the CAH; or
- the facility provided medical nutrition therapy (MNT) services.
A CAH is a specific designation given to hospitals in rural census tracts that comply with other geographic criteria. A CAH must also maintain certain size and care standards. If an institutional facility does not satisfy either of these requirements, it may not submit telehealth reimbursement claims.
Unauthorized Originating Site: There were three unallowable claims because the patients received care at an unauthorized originating site. Two patients received services at their residences while the other received services at an independent renal dialysis clinic. The eight types of authorized originating sites are defined as follows:
- Office of a physician or practitioner
- Critical access hospital
- Rural health clinic
- Federally qualified health center
- Hospital
- Hospital-based or critical access hospital-based renal dialysis center (including satellites)
- Skilled nursing facility
- Community mental health center
Ineligible Telecommunication Systems: There were two unallowable claims because the provider did not use an interactive telecommunications system, which requires at least the capability for two-way, real-time communication between provider and patient. Telephones, fax machines, and emails do not satisfy this definition. There is an exception, however, for asynchronous technologies for providers in Alaska and Hawaii. One claimant using an asynchronous technology was not located in either of those two states while the other used a telephone to provide services.
Noncovered Services: One claim was unallowable because it was for a noncovered service. The claimant rendered psychotherapy services which were not reimbursable expenses at the time. The CMS website maintains a list of all covered services and their corresponding billing codes.
Physician Location: One claim was unallowable because the practitioner was located outside the United States. Medicare generally requires a physician to be located in the United States when providing care. In this case, the physician was located in Pakistan.
II. Causes of Unallowable Claims and Recommended Actions
The OIG identified three fundamental causes that resulted in unallowable claims:
- Medicare Administrative Contractors (MAC) could not edit billing inputs for unallowable originating sites because the claim form did not have a field to input the originating-site location.
- MACs did not implement the claim edits described in The Medicare Claims Processing Manual, particularly Chapter 12, §190.7, which requires MACs to
- install edits to ensure that only properly licensed practitioners are paid for covered telehealth services;
- deny services billed with a telehealth modifier if the procedure code is not a covered telehealth service; and
- deny payment for distant-site claims from institutional facilities, except MNT services, unless the distant site is a CAH that has elected the Method II payment option, and the practitioner has reassigned his or her benefits to the CAH.
- The practitioners were not aware of telehealth-specific reimbursement requirements. Even though CMS provides guidance, it does not offer practitioner training on telehealth services, which in turn contributes to the lack of industry awareness.
The OIG recommended that CMS take the following actions to remedy the underlying causes of unallowable claims:
- Conduct periodic post-payment reviews and disallow payments for claims that do not conform to CMS guidelines.
- Improve communication with MAC’s to ensure proper implementation of claim edits listed in the Medicare Claims Processing Manual.
- Implement practitioner training programs on Medicare telehealth requirements.
Following up on the OIG’s report, the Department of Health & Human Services announced last November that it would perform a similar review of telehealth claims submitted to state Medicaid programs. The increasing scrutiny of regulators should encourage providers to take appropriate steps to ensure they are complying with all applicable federal and state requirements for telehealth reimbursement claims. Even so, navigating the complex environment of Medicare reimbursement policies can be challenging. If you need any assistance with telehealth or other Medicare issues, feel free to contact Andrew Johnson (513-651-6814 or aojohnson@fbtlaw.com) of Frost Brown Todd’s Health Care Service Team.

